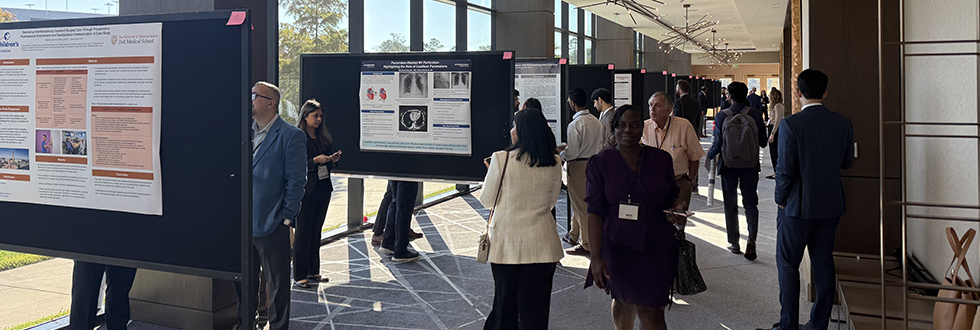
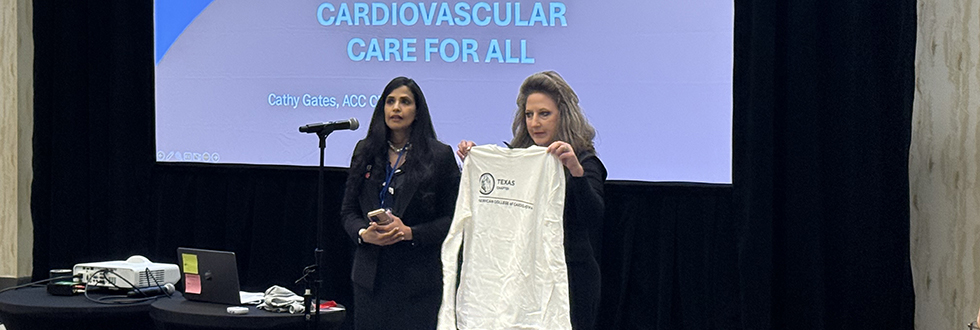
Thank You for Attending the 2025 TCACC Annual MeetingThank you to everyone who joined us in Houston for the 2025 TCACC Annual Meeting. Your participation helped make the meeting a meaningful experience for cardiovascular professionals across Texas. 2025 Annual Meeting Recap
Save the Date: 2026 Annual MeetingSave the date for the 2026 TCACC Annual Meeting, October 17–18, 2026, in San Antonio, Texas, at the Westin Riverwalk. Program and registration details will be shared soon. Learn MoreWhy Join TCACC?Join a powerful network of cardiovascular professionals committed to advancing heart health through the Texas Chapter of the American College of Cardiology. As a member, you can access exclusive resources, discounted education, career opportunities and make meaningful connections that strengthen your impact. Whether you're building your expertise or expanding your reach, TCACC is here to support your journey. Explore Our MembershipJoin. Share. Impact.Get involved and help shape the future of cardiology in Texas. TCACC sections connect you to exclusive education, advocacy tools, leadership opportunities and a statewide network of peers who share your passion. With over 20 sections to choose from, there's a place for every interest and specialty. Ready to make an impact? Volunteer for a section or submit content to share your voice and expertise. Find Your Section |